Working in healthcare has always been associated with a mission. With help, responsibility, dedication and a sense of meaning that goes beyond most professions. Plato, the Greek philosopher, writing “No physician, if he is a true physician, cares not for his own benefit, but for the health of the sick”, used the physician as a model example of a good craftsman, that is, one who does not work for profit, but for the good of the one whom he serves. This quote indicates that as early as the 4th century BC there was an idea of ethical professionalism, in which job satisfaction comes not from profit, but from the realization of the good of the other person. And although this is a coherent and objectively correct vision in today's medical age, it can cause a one-sided perception of the profession. Increasingly, there are voices of frustration, fatigue and discouragement among doctors. Modern medicine is faced with a paradox: those who save others are increasingly in need of support themselves. Doctor, doctor, does anyone ask you how you feel at work?
Job satisfaction is a concept that has both an emotional and cognitive dimension. The classic definition of Edwin Locke (1976) defines it as “a positive emotional state resulting from the evaluation of one's own work or its experiences” **. Paul Spector adds that it is “the set of attitudes of the employee towards different aspects of his work”, such as salary, relationships, autonomy or development [3].
In the case of medical professions, job satisfaction is of a special nature. It results from a combination of internal factors, such as appointment, ability to provide assistance, contact with the patient, and external factors related to the system, work organization and institutional conditions. For doctors, the elements of professional identity are also crucial, i.e. sense of meaning and security, patient trust, decision-making autonomy and the quality of the professional relationship. When these areas are shaken, even with a good salary, satisfaction decreases, and with it motivation and mental resilience.
Prior to the COVID-19 pandemic, the topic of physician satisfaction and well-being was considered primarily as an issue of individual psychological resilience (“resilience”), rather than as a systemic responsibility. While the literature prior to 2020 was dominated by works that treated burnout as a personal problem of the doctor, the pandemic crisis made visible the key role of organizational determinants of the mental health of personnel. The professional well-being of health workers ceases to be seen as a “soft indicator”, it becomes a fundamental element of quality and safety in the health system. In other words, the satisfaction of doctors today is an indicator of the stability of the entire system.
WHO Report Mental Health of Nurses and Doctors in the EU, Iceland and Norway (MenD, 2025) is the first ever study of such a wide scope - it covered more than 90 thousand doctors and nurses from 29 European countries, including Poland. The results are alarming: one in three doctors and nurses surveyed showed symptoms of depression or anxiety, and one in ten declared suicidal thoughts [4]. Less than 70% of staff describe themselves as “job satisfied” and the average well-being rate (WHO-5) in this group is one-third lower than in the non-health care population [4]. The study clearly showed that organizational factors: excessive hourly load, lack of influence on the work schedule, staff shortages and lack of support from superiors, have a stronger influence on satisfaction and mental health than personal factors [4]. These are signs that the system has for years expected more from people than it can handle without real support.
The OECD and WHO data confirm that Poland is in the group of countries with the highest rate of workload of medical personnel in Europe, with a simultaneous shortage of personnel [5]. In such conditions, job satisfaction ceases to be an “addition” to the mission, and a prerequisite for patient safety, quality of care and durability of the entire system.
Measuring job satisfaction has been the subject of scientific research for years, not only for diagnostic purposes of the psychological well-being of doctors, but also as a predictive value of negative phenomena: staff turnover, burnout, decline in the quality of care and monitoring the effectiveness of interventions. In the medical environment, four main methods are used:
This is the most commonly used method. Responses are measured on fixed scales, and the results can be analyzed statistically. Below is a summary of the most commonly used tools.
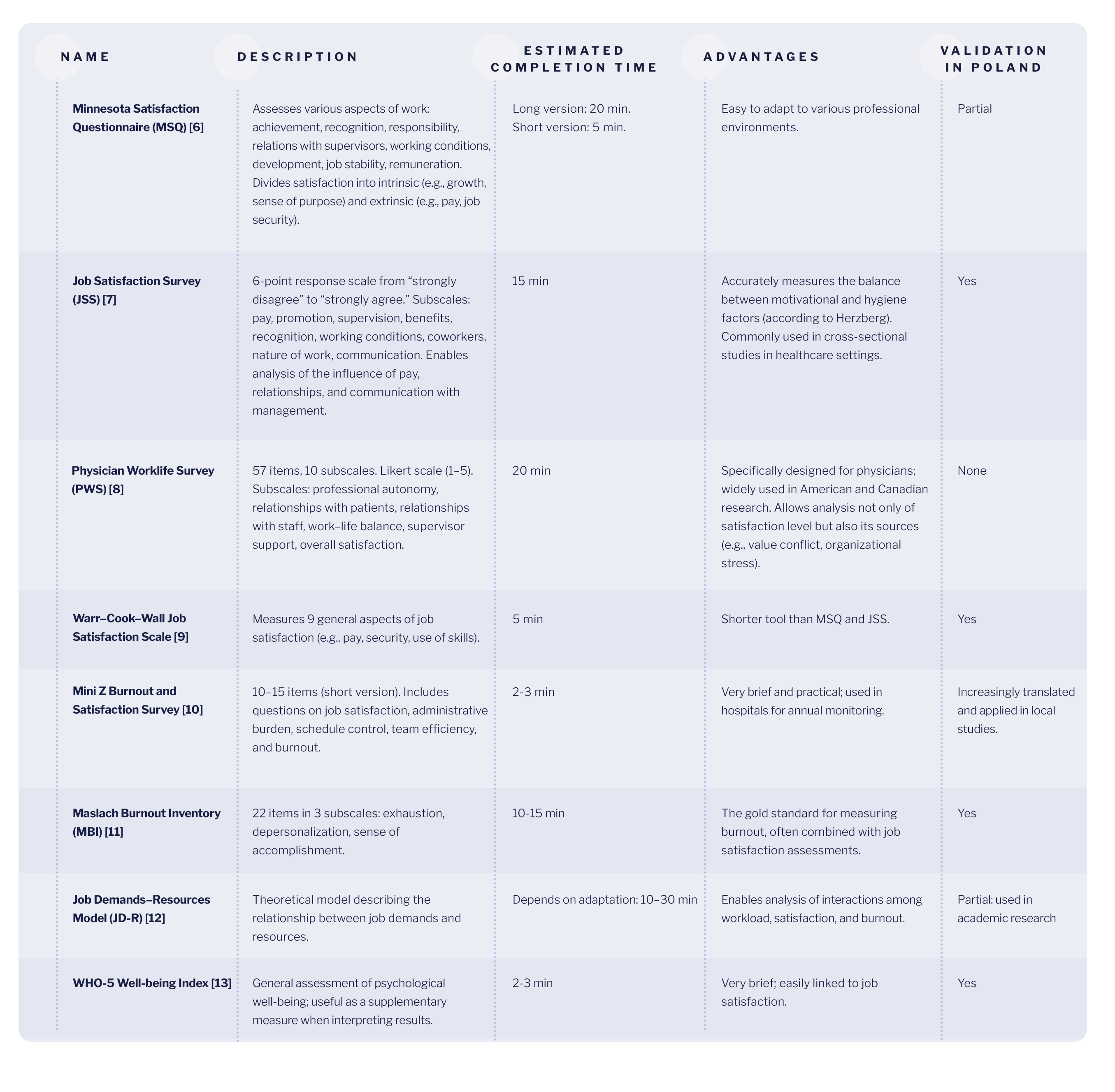
In Poland, there is still a lack of a uniform tool for monitoring the professional satisfaction of doctors on a national scale. In environmental studies, author's questionnaires inspired by MSQ or JSS are mainly used, usually consisting of 10-20 questions.
In recent years, scientists have increasingly turned to qualitative methods, especially when they want to understand**why people feel satisfaction with the profession (or lack thereof), and not only to what extent.
Molds:
Increasingly, job satisfaction is analyzed indirectly, through measurable indicators that correlate with employee satisfaction. This is a particularly popular approach in hospital management.
Examples of indicators: [17] [18] [19] [20]
The advantage of this solution is objectivity and ease of monitoring over time, which can be useful in the context of analysis of improvement or deterioration. The main limitation, however, is that the above indicators do not speak why employees are (not) satisfied, they only signal a trend that needs to be deepened with qualitative research.
The most valuable projects combine survey and interviews. Thus, it is possible to analyze both “who” (how many people are dissatisfied), and “why”. This approach gives the most complete picture, combining the precision of numerical data with the depth of interpretation of answers in conversations.
Increasingly, organizations are implementing modern “live” measurement methods:
Short surveys (usually 5—15 questions) sent periodically (weekly, monthly, quarterly) to monitor moods and changes over time. They allow you to record current emotions and evaluate working conditions in real time, instead of waiting for annual satisfaction surveys. In the healthcare sector, such technologies can be particularly valuable because workers are exposed to rapid shifts, heavy workloads, shifts, so more frequent mood monitoring can help catch problems before they escalate into burnout or turnover.
Sentiment analysis is a method of determining employment-related sentiment. Employee “moods” and employee engagement are two related but different aspects of work experience. Mood refers to emotions and feelings towards work, the team and the organization, that is, how people feel in the workplace and what atmosphere prevails in the organizational culture. Commitment describes the level of attachment and motivation towards the goals of the organization, that is, how much employees want to act, initiate ideas and take responsibility. Sentiment analysis is the use of AI/NLP (natural language processing) algorithms to process open text responses, comments, intranet entries or instant messengers to extract emotions, tendencies and concerns of employees (“I feel overworked”, “lack of support”) to seek a deeper analysis of the causes of low satisfaction.
In practice, such methods are rarely used in Polish hospitals and clinics, often infrastructure, budgets and privacy issues are a barrier, but also education and awareness about the possibilities. The solutions are only in the pilot phase, mainly used in private medical networks or research projects.
Studies show that high hourly workload, too many patients, administrative responsibilities and poor organizational conditions significantly reduce the satisfaction of doctors. A 2017 Dutch study found that “heavy workload” was associated with significantly lower job satisfaction among doctors, while 35% of participants would like to work fewer hours [24].
A sense of autonomy in clinical decision-making and influence on work organization is one of the strongest factors of job satisfaction. In an analysis conducted among physicians in East Asia, professional autonomy was identified as one of the main elements conducive to job satisfaction [25]. Systematic reviews confirm that greater control over one's responsibilities (“job control”) protects against burnout and decreased satisfaction [26].
The culture of the workplace, the quality of relationships with colleagues and superiors, the support of the team — all this has a significant impact on the satisfaction of doctors. In a European analysis, 11 out of 12 studies found that greater support from colleagues and a positive team atmosphere correlate with higher satisfaction [27]. In the literature, the quality of management and leadership is also emphasized as an element of organizational conditions.
According to Herzberg's classical theory, remuneration is not a motivating factor in the strict sense, but a “hygiene factor” - its lack leads to dissatisfaction, while an adequate level does not automatically guarantee an increase in satisfaction. In the context of the medical profession, this means that financial stability is a necessary but not sufficient condition for professional well-being. Doctors expect not only fair remuneration, but also a sense of meaning, influence and recognition, that is, elements that already belong to the group of motivational factors. Research confirms that only when stable financial conditions are combined with a sense of autonomy and development, does it lead to a sustained increase in job satisfaction [25] [27].
Job satisfaction increases when doctors have access to training, professional development programs, and clear career paths. A review of the European research literature indicates that development opportunities promote a sense of purpose, increase engagement and reduce the risk of staff turnover. For younger doctors, this is often a key factor in staying in the profession [27].
Maintaining a balance between work responsibilities and personal life is now one of the most important determinants of professional well-being. Studies conducted in Western European countries have shown that the difference between actual and preferred working hours significantly affects the level of satisfaction [24]. Comparative analyses also indicate that work—family conflict is one of the main factors in the decline in job satisfaction and burnout [27].
Improving job satisfaction is not a matter of a single intervention. It requires an integrated approach combining individual, organizational and systemic actions. As highlighted by the WHO report Mend (2025), initiatives focused solely on individual resilience are ineffective if they are not accompanied by structural changes in the workplace [4].
The most comprehensive analysis to date of the effectiveness of individual interventions, published in The American Journal of Medicine (Haslam et al., 2024) showed that individual-directed (physician) programs lead to small, though statistically significant, changes in occupational burnout [28]. However, the authors emphasized that the effects are usually short-lived and dependent on organizational support [28].
Solution: Introducing direct-to-physician programs aimed at improving their well-being, from mindfulness training and stress management workshops to coaching and psychological interventions. Individual interventions are therefore an important element of burnout prevention, but effective only if they are accompanied by an appropriate work structure, support from superiors and an organizational culture conducive to well-being.
By far the strongest influence on the satisfaction of doctors is the changes in work organization and personnel management. According to the report American Medical Association (AMA) of 2023, 48.2% of physicians reported symptoms of burnout, and the main causes were excessive administrative responsibilities and lack of support from the medical team [29]. In addition, the results of another analysis indicate that in wards with a higher staffing rate and a lower burden of patients on the doctor, there was a 25— 40% lower level of burnout and a significantly higher level of job satisfaction [30].
Solution: Reducing the administrative burden on doctors by delegating tasks and standardizing documentation can significantly improve their job satisfaction. Efficient documentation management is also crucial. From the study JAMA Network Open (2024) it follows that doctors who have used simplified data recording tools (among others. voice modules and automatic form filling), spent less time on administrative matters, which directly translated into a higher sense of efficiency and a better work-life balance [31].
Doctors are happier when they work in an environment based on trust, openness, and co-decision making.
Solution: The use of a participatory leadership style, oriented towards dialogue, mentoring and sharing of responsibility. Regular, constructive feedback and the feeling that the employee's voice matters in the decision-making process is key.
Digitalization of the healthcare system can be both a source of frustration and a powerful support. The quality of the implementation and training of personnel is crucial. Poorly designed EHR (Electronic Health Records) systems generate excess clicks, errors, and cognitive overload [32].
Solution: Well-tailored solutions, such as integrated instant messaging, automated documentation generation or AI-based assistants, can reduce uptime by up to 25-30% [31].
Regular training in the use of digital tools and AI is an important factor in the successful use of technology. Research by the American AMA has shown that physicians need a reliable, practical source of knowledge in the field of AI and new documentation systems [33]. Training should cover not only the use of tools, but also the basics of interpreting AI results, data security and ethical aspects of its use [33].
One of the main sources of professional fulfillment for doctors is the sense of impact and meaning that grows when they can observe the effects of treatment. Maintaining contact after the visit promotes better follow-up and at the same time deepens the doctor-patient relationship.
Solution: The use of tools that allow the doctor to be in constant contact with the patient, such as secure digital communication platforms or health monitoring applications.
Effective communication within the medical team has a direct impact on the well-being of the staff. Joint team meetings, feedback culture and mentoring improve trust and reduce the risk of burnout.
Solution: implementation of encrypted internal messengers and reporting standards.
The satisfaction of doctors is the key to the quality of care and patient safety. It requires a balance between workload, organizational support and thoughtful use of technology. The conclusions of the WHO report coincide with the findings of the scientific literature, which for years has identified workload, lack of autonomy and poor communication as the main sources of dissatisfaction among doctors [4]. The World Health Organization recommends that improvements in job satisfaction should not be limited to individual intervention programs, but should include structural changes: flexible scheduling of shifts, protection of rest time, zero tolerance for violence in the workplace and regular monitoring of the mental health of staff [4].
In this context, they take on special importance modern communication tools, not as a source of additional duties, but as Support infrastructure. WHO points out that digital technologies can improve the well-being of doctors when they serve a better organization of work and facilitate teamwork, rather than control or bureaucracy.
Examples are safe medical communicators or asynchronous patient communication systems that reduce time pressure, reduce stress and increase the sense of meaning in work. For clinical practice, this means shifting the focus: from “coping” with burnout to designing a work environment that supports satisfaction. An investment in the well-being of staff is an investment in the health of the entire system.
If you want to look deeper into the subject of physicians' well-being - we have prepared an e-book based on data and experiences from everyday practice. E-book you can download here and return to it at a convenient time.